If your knee is injured, through either trauma or arthritis, performing everyday activities such as walking, climbing stairs, and even lying down, may cause some pain. If you have tried and exhausted all conservative treatment options such as medications, walking aids and physical therapy, then you may need to consider knee replacement surgery.
This type of surgery is a safe and effective reconstructive procedure that will enable you to resume activities that you are no longer able to. If you are looking to get back to your daily routine as quickly as possible, you may want to consider a knee replacement. Coffs Harbour residents can contact the team at Mid North Coast Hip & Knee Clinic today for more information.
What causes the need for a knee replacement?
A knee replacement, may be recommended if the knee joint is worn, damaged, or stiff, and prevents you from carrying out your typical daily activities. If you have any of the following, then a knee replacement surgery may be of benefit to you:
- Osteoarthritis with severe pain and stiffness
- Deformity of the knee joint and instability
- Chronic rheumatoid arthritis and pain
- Previous traumatic knee injury
Am I a candidate for a knee replacement procedure?
A suitable candidate for a knee replacement surgery will usually meet the following criteria:
- Severe knee pain or stiffness prevents you from carrying out your regular day-to-day activities such as walking up the stairs, sitting and getting up out of chairs, and walking.
- Knee pain is continuous throughout the day and night, even while you sleep.
- Knee inflammation and swelling around the joint that does not improve with anti-inflammatory medications.
- Deformity and instability at the knee joint.
- Detrimental effects on mental health as a result of knee pain and inability to contribute to social activities.
- Your current knee replacement is in need of a revision replacement
If you have exhausted all other non-surgical treatment options, then knee replacement surgery may be the treatment of choice for you.

Using state-of-the-art equipment we can comprehensively analyze your knee joint to provide the treatment tailored to you.
The difference
between a partial
knee replacement
and a total knee replacement
The severity of your condition will determine whether you require a partial or total knee replacement:
Partial Knee Replacement
If your condition has been diagnosed early and the arthritic damage to your knee is not too severe, you may be eligible for a partial knee replacement. In this instance the disease has not progressed to all 3 compartments of the arthritic knee, allowing the surgeon to replace fewer parts.
Total Knee Replacement
If you are suffering from severe arthritic knee pain or chronic knee inflammation, it is likely you may need a total knee replacement. All 3 major compartments of the knee may need to be replaced. Knee replacement prostheses are most commonly made of metal alloys, usually, titanium or cobalt-chromium based. Some implants are made of ceramics or ceramic/metal mixtures.
What is a knee replacement made of and how is it fixed in place?
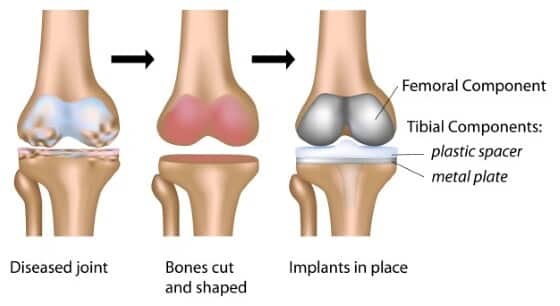
Total knee replacement prostheses are most commonly made of metal alloys, usually titanium or cobalt-chromium based. Some implants are made of ceramics or ceramic/metal mixtures. The spacer between the femoral and tibial component, and patella resurfacing component, is made of ultra-high molecular weight polyethylene. The components may be fixed to the femur and tibia with or without bone cement. Cement fixation, particularly on the tibial side of the joint, is known to have a reduced rate of revision.

How is total knee replacement surgery carried out?
Our team of experts will guide you through your surgery from your initial consultation, all the way through to your post-operative care:
Consultation
During your consultation, we will discuss your medical history, inspect your knee and your X-rays and may take some blood tests. We will talk you through the procedure and give you the opportunity to ask any questions you may have.
Procedure
A total knee replacement involves replacing the main joint surfaces at the end of your thigh bone (femur) and shin bone (tibia). It may also involve resurfacing the kneecap (patella) with a plastic dome. The main steps of a knee replacement are:
- Damaged cartilage and bone are removed to prepare the joint for replacement.
- Once removed, the cartilage and damaged bone are replaced with a prosthetic. These parts are used to recreate the surface of the joint and are either cemented or fixed in place.
- If the patella is damaged, the undersurface will be replaced with a plastic dome.
- A spacer is then inserted between the new components to allow for smooth gliding.
Recovery
Whilst every patient has a different starting point prior to knee replacement, patients recover better when they are well informed and have undergone a period of physiotherapy with strength and conditioning prior to surgery. Patients are encouraged to walk almost immediately following surgery under the supervision of a physiotherapist. It takes approximately 2 weeks for the skin wound to be well healed and it may be wet after that.
Most knee replacement patients will have returned to driving a car within 6 weeks. There will be a steady improvement over the first 3 to 4 months but it’s not unusual to still require some simple pain relief during this time. The knee replacement may remain swollen and warmer than the other side for up to 12 months after surgery but this is normal. Overall recovery for a total knee replacement can be up to 18 months.
Benefits of knee replacement surgery
There are a number of significant benefits of having knee replacement surgery:
- Relieve pain
- Correct leg deformity
- Restore knee movement
- Improved mobility
- Resume your regular everyday activities
Severe inflammatory disorders are one of
the main causes of having a knee replacement.

The overall recovery time after knee
replacement surgery can be up to 18 months.
Are there any risks associated with a knee replacement?
Any surgical procedure carries risks, but when carried out by a highly experienced professional like Dr Broadhead, it’s considered a safe and effective procedure. Unlikely risks associated with a knee replacement include:
- Deep venous thrombosis (DVT)
- Infection
- Fracture
- Loosening
How much does a knee replacement cost?
The cost of knee replacement in Australia varies widely, depending on whether treatment occurs in a public or private hospital and the level of cover provided by private health insurance. Treatment at a public hospital is fully covered by Medicare. For treatment at a private hospital, our staff will be able to provide you with a quotation, taking into account your level of health insurance coverage.
If you do not have private health insurance but still wish to be treated in a private hospital, you will be provided with a full fee estimate, including fees for the surgeon, surgical assistant, anaesthetist, the private hospital and any required surgical implants or prostheses.

Why choose us for your knee replacement procedure?
At the Mid North Coast Hip & Knee Clinic, we pride ourselves on providing patients with the highest standard of care in the treatment of orthopaedic trauma and all hip and knee disorders. We have years of experience treating patients of all ages from all along with the Mid North Coast and surrounding communities, using a multi-disciplinary approach, working together to form a comprehensive and patient-specific treatment plan.
Our Experts
Our team of dedicated professionals at The Mid North Coast Hip & Knee Clinic take the time to understand your condition and how it impacts your life. With a range of medical specialists and allied health professionals, we take pride in guiding you along your treatment journey. Find out more about our experts below:

Dr Matthew
Broadhead
Orthopaedic Surgeon | BSc(Med) MBBS(Hons) ChM PhD FRACS FAOrthA
Dr Matthew Broadhead is a Fellowship-trained Australian Orthopaedic Surgeon who specialises in lower limb reconstruction and the treatment of traumatic, degenerative and inflammatory disorders of the hip and knee.

Mihai
Mitrache
Principal Physiotherapist,
Active Physiotherapy and Wellness
Mihai Mitrache is the Principal Physiotherapist at Active Physiotherapy and Wellness. He has a subspecialty interest in hip and knee rehab and additional experience in the management of chronic pain.

Dr Sridhar
Vijayan
Musculoskeletal
Physician
Dr Sridhar Vijayan is a Physician with vast experience in musculoskeletal medicine, having worked in Trauma & Orthopaedics both in the UK and Australia.

Dr Su-Yin
Yeong
General Practitioner, Chronic
Pain and Integrative Medicine
Dr Su-Yin Yeong graduated with a Bachelor of Medical Studies and Doctor of Medicine from the University of NSW in 2013. She is a Fellow of the Royal Australian College of General Practitioners.

Dr Karen
Wong
Consultant
Anaesthetist
Dr Karen Wong is an Australian Fellowship-trained Consultant Anaesthetist with a focus on caring for patients undergoing hip and knee replacement surgery.

Dr Angela
Suen
Consultant
Anaesthetist
Dr Angela Suen is an Australian Fellowship-trained consultant anaesthetist with a particular interest in caring for patients undergoing orthopaedic surgery.
Our Locations
You can find us at a number of locations across the Mid North Coast:
Coffs Harbour
Coffs Harbour Specialist Centre
Suite 203, 343 Pacific Hwy,
Coffs Harbour NSW 2450
Coffs Harbour
Coffs Harbour Health Campus
345 Pacific Hwy,
Coffs Harbour NSW 2450
Coffs Harbour
Baringa Private Hospital
31 MacKays Rd,
Coffs Harbour NSW 2450
Taree
Mayo Private Hospital
Specialist Consulting Suites
2 Potoroo Dr, Taree NSW 2430
Forster
Forster Private Hospital
Specialist Consulting Suites
5A South St, Forster NSW 2428
Sydney
North Shore Private Hospital
3 Westbourne St
St Leonards NSW 2065
Sydney
Prince of Wales Private Hospital
Barker St
Randwick NSW 2031
How to schedule the exploratory consultation?
Please discuss with your General Practitioner and organise a referral, then contact reception to book your initial consultation. to Dr BroadheadContact us today to book your initial consultation via phone or online. At your first appointment you will need to bring the following:
- Medicare card, DVA card, Pension card
- Health insurance details
- Worker compensation claim number
FAQs
If you still have some questions or concerns regarding a knee replacement, then please don’t hesitate to contact us. In the meantime check out the section below for some additional information:
Can I have a knee replacement if I have had previous surgery?
If you’ve had previous knee surgery, it won’t stop you from having a knee replacement. However, the choice of prosthesis used by your surgeon may vary.
How can I prepare my home for recovery?
Here are several tips to help you ready your home for your recovery:
- Clean and remove all clutter and tripping hazards
- Install fall-prevention equipment
- Prepare a rehabilitation and physio area
- Sleep downstairs until you can walk upstairs comfortably
How long will the total knee replacement last?
On average the knee implants used for a knee replacement last about 15 to 20 years. However, age is a major factor in determining how long a total knee replacement will last. Males also have a higher rate of revision than females.
What is the best age to have a knee replacement?
Most knee replacement patients are between 50 to 70 years. However, patients over the age of 70 can also benefit from the procedure.
Is a knee replacement a major operation?
A knee replacement is a major operation and is only recommended if other treatment options haven’t helped to relieve pain or improve mobility.
How painful is a knee replacement?
As the surgery is carried out using anaesthesia, you won’t feel any pain during the operation. However as with any surgery, after the procedure, you’ll feel some discomfort but this is normal.
If you suffer from a knee or hip condition,
we can help you get back to life.
Pain and discomfort caused by orthopaedic conditions affect our patients negatively every day.
Which is why we work so hard to provide relief for every one of our patients. Our team is highly
trained in the diagnosis, treatment and management of all musculoskeletal conditions and injuries.











