What is a hip replacement?
A hip replacement is a safe and effective reconstructive surgery that may be suitable for patients with hip pain who have responded poorly to conservative treatments. It aims to relieve pain in patients who have sustained a traumatic injury or have advanced arthritis in the hip joint.
If your hip joint has been damaged by progressive arthritis, a fracture, or an underlying condition, you may require a hip replacement. You can contact the team at Mid North Coast Hip and Knee Clinic to book an initial consultation or to find out more information.
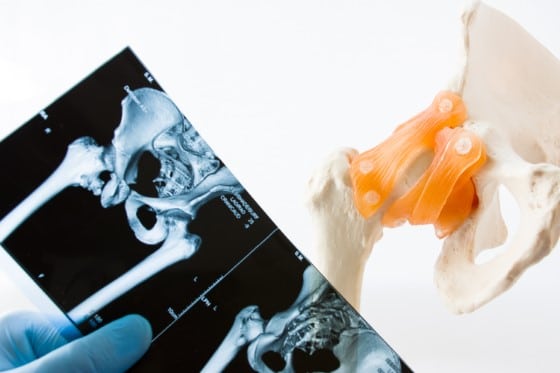
A hip replacement is a procedure during which your orthopaedic surgeon replaces the “ball and socket joint” of your hip with an artificial prosthesis. The prostheses are most commonly made of metal alloys, usually, titanium or cobalt-chromium based. Some implants are made of ceramics or ceramic/metal mixtures.
The spacer between the femoral and tibial component, and patella resurfacing component, is made of ultra-high molecular weight polyethylene. The components may be fixed to the femur and tibia with or without bone cement. Cement fixation, particularly on the tibial side of the joint, is known to have a reduced rate of revision.
What causes the need for a hip replacement?
Hip replacement surgery may be recommended when presenting with any of the following:
- Hip pain that stops you from carrying out typical daily activities
- X-rays displaying hip joint degeneration
- Overnight stiffness and pain
- Failed non-surgical therapy
Am I a candidate for hip replacement surgery?
The most common cause of stiffness and hip pain that warrants the need for hip replacement surgery is osteoarthritis – an arthritic condition that causes pain and stiffness in your hip joint and other areas of the body.
The following conditions may make you a suitable candidate for a hip replacement:
- Continuous pain that prevents you from carrying out your normal daily activities such as walking, going upstairs, and regular exercise.
- Pain that is unrelieved by pain relief medications and continues day and night.
- You experience regular stiffness and swelling around your hip joint.
- Hip fracture
What is the hip replacement
made of and how
is it fixed in place?
There are many different designs of hip replacement prostheses. The main differences between the prostheses are the way in which they are fixed to the bone and the bearing surfaces.
Hip replacement prostheses may be classified as:
- Uncemented – both femoral and acetabular components rely on a tight fit for initial bone fixation. The bone grows onto the components for long term fixation.
- Hybrid – the femoral component is fixed inside the femur with bone cement and the acetabular component relies on bone growth for fixation.
- Cemented – both the femoral and acetabular components are fixed in place with bone cement.

This metal or ceramic ball is attached to the top of your femur.

During a total hip replacement, an orthopaedic surgeon replaces the “ball and socket joint” of your hip, with an artificial prosthesis.
How is hip replacement surgery carried out?
If you choose to have your hip replacement with us, you can expect the following:
Consultation
During your consultation, we will talk you through the whole procedure and give you the opportunity to ask any questions you may have. We’ll also discuss your medical history in detail, inspect your hip and any X-rays and if necessary, we’ll also request some blood tests.
Procedure
During a total hip replacement, your orthopaedic surgeon will remove the damaged segments of your hip and replace them with artificial prostheses. The femoral head is replaced with a metal stem that’s placed into the centre of the thigh bone. A metal or ceramic ball is then attached to the head of the stem, acting as the new femoral head.
The damaged surface of the “socket” (acetabulum) is then removed and replaced with a metal one, secured in place using cement or screws. A spacer called a liner is then inserted between them to allow for smooth gliding and to facilitate hip movements.
Recovery
Whilst every patient has a different starting point prior to hip replacement, relief from arthritic hip pain is usually very rapid. Patients are encouraged to walk almost immediately following surgery under the supervision of a physiotherapist.
It takes approximately 2 weeks for the skin wound to be well healed and it may be wet after that. Hip replacement patients can normally have returned to driving a car by 6 weeks, after being approved by the surgeon. After a rapid improvement in the first three months, progress will start to plateau, and you will return to normal activity levels.
Benefits of hip replacement surgery
Hip replacements are one of the most common and most successful forms of treatment of osteoarthritis of the hip. They provide significant improvements in range of motion and a remarkable reduction in pain. The numerous benefits include:
- High success rates
- Pain relief
- Improved mobility
- Long-lasting relief
- Better quality of life

Physiotherapy allows you to get used to any new movements your new hip has to go through and increases your chances of returning to normal function.
Are there any
risks associated
with a hip
replacement?
Any surgical procedure carries risks, but when performed by a highly experienced orthopaedic surgeon like Dr Broadhead, it’s a very safe and effective procedure. Unlikely but potential risks include:
- Deep venous thrombosis (DVT)
- Infection
- Fracture
- Dislocation
- Change in leg length
- Loosening
How much does a hip replacement cost?
The cost of a hip replacement varies widely, depending on whether treatment occurs in a public or private hospital, along with the level of cover provided by any private health insurance. Treatment at a public hospital is fully covered by Medicare and any for treatment at a private hospital, our staff will be able to provide you with a quotation.
If you do not have private health insurance but still wish to be treated in a private hospital, you will be provided with a full fee estimate including fees for the surgeon, surgical assistant, anaesthetist, the private hospital and any required surgical implants or prostheses.

Why choose us for your hip replacement procedure?
At the Mid North Coast Hip & Knee Clinic, we pride ourselves on providing patients with the highest standard of care. Our team of dedicated professionals take the time to understand your condition and how it impacts your life. We treat patients of all ages using a multi-disciplinary approach, working together to form a comprehensive and patient-specific treatment plan.
How to schedule a consultation?
Please discuss with your Doctor to organise a referral, then contact reception to book your initial consultation. Please have available at the time of booking:
- Medicare card, DVA card, Pension card
- Health insurance details
- Worker compensation claim number
FAQs
If you still have some queries or concerns regarding our hip replacement treatment, then check out the section below for additional information:
When can I go home after hip replacement surgery?
Most hip replacement surgeries are performed on an impatient basis, meaning that you typically have to stay in the hospital between 3-4 nights before your discharge.
When can I drive after hip replacement surgery?
Six weeks normally or once approved by the surgeon.
How long will the hip replacement last?
In 2019, the Australian Orthopaedic Association National Joint Replacement Registry (AOANJRR) reported the overall revision rate of primary total hip replacement as 11.7% at 18 years after surgery.
If you suffer from a knee or hip condition,
we can help you get back to life.
Pain and discomfort caused by orthopaedic conditions affect our patients negatively every day.
Which is why we work so hard to provide relief for every one of our patients. Our team is highly
trained in the diagnosis, treatment and management of all musculoskeletal conditions and injuries.











